Clinical trials always pose a challenge to demonstrating a drug’s safety and efficacy. Sometimes, the challenges are beyond difficult, presenting situations where it isn’t ethical or feasible to demonstrate efficacy in humans.
Consider the following scenarios (which have occurred):

A bioterror attack with people exposed to a dangerous disease (anthrax, plague, Ebola)
A natural hazard with potentially fatal consequences (snake or insect bite)


A casualty event with people exposed to radiation, cyanide, or nerve agents
How can countries prepare for medical emergencies like this?
Preparing for these emergencies requires developing both preventatives and treatments (i.e., medical countermeasures). But – how can the efficacy of medical countermeasures be demonstrated? These emergencies aren’t predictable, so a clinical or field trial is not a viable strategy. Conducting a challenge trial that deliberately exposes human volunteers to lethal or permanently disabling toxic biological, chemical, radiological, or nuclear substances is unethical.
Two sections of the Code of Federal Regulations (CFR) provide a mechanism to support developing countermeasures in these situations:
Within the United States, these regulations support developing treatments without the need for efficacy studies in humans. They are colloquially referred to as “The Animal Rule”.
These are regulations and present legal requirements for approval. This differs from a guidance document like Product Development Under the Animal Rule, which describes the FDA’s current thinking on animal rule requirements but is not legally binding.
Focusing the nation’s attention on bioterrorism
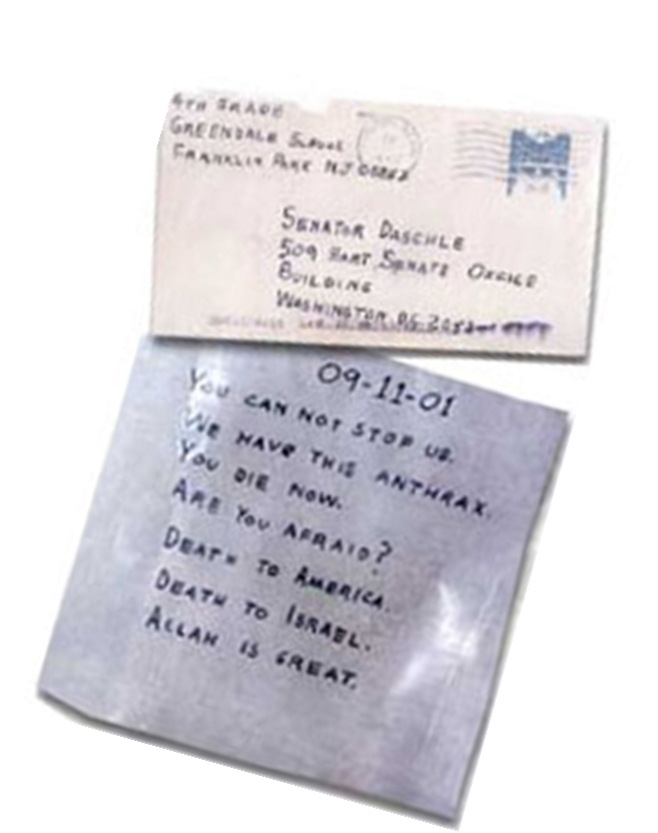
In 2001, anthrax spores were sent through the US mail. Senators and news media were targeted by the terrorist attack. Many people including US mail carriers were exposed. 22 cases of anthrax infection occurred, and 5 people died. Tens of thousands of people were potentially exposed and because of the nature of anthrax spores, they each required extensive post-exposure prophylactic treatment (60 days of antibiotics). The animal efficacy rule was first published for comment in 1997, but the 2001 anthrax incident focused attention on a regulatory pathway that did not include demonstration of efficacy in humans prior to approval.
Drug development under the Animal Rule
Approval of medical countermeasures under the Animal Rule doesn’t eliminate the need for clinical trials entirely. Any agent developed under the Animal Rule must demonstrate safety in humans. However, the efficacy data comes from well-controlled studies using animal models.
Four basic tenants must be met for a countermeasure to qualify for development under the animal rule:
- There must be a reasonably well-understood pathophysiological mechanism of the toxicity of the substance and its prevention or substantial reduction by the product;
- The effect is demonstrated in more than one animal species expected to react with a response predictive for humans, unless the effect is demonstrated in a single animal species that represents a sufficiently well-characterized animal model for predicting the response in humans;
- The animal study endpoint is clearly related to the desired benefit in humans, generally the enhancement of survival or prevention of major morbidity; and
- The data or information on the kinetics and pharmacodynamics of the product or other relevant data or information, in animals and humans, allows selection of an effective dose in humans.
To date, the FDA has approved 17 products using the animal rule. CDER has approved 13 products covering a range of indications including nerve gas, radiation and cyanide exposures, and diseases (pneumonic and septicemic plague, anthrax, and smallpox). CBER has approved four interventions (botulinum toxin, anthrax treatment, and 2 post-exposure prophylaxis anthrax treatments). You can read about how my Certara colleagues have supported the approval of some of these products in this blog.
Once an approval is granted, it is likely to come with additional commitments that can include:
- Post-marketing studies to evaluate safety and clinical benefit if circumstances arise in which a study would be feasible and ethical. A plan or approach to conducting such a study must be included with the marketing application.
- The approval will have restrictions to ensure safe use if needed.
- Information must be provided to patient recipients explaining that for ethical or feasibility reasons, the product’s approval or licensure was based on efficacy studies conducted in animals alone.
The Animal Efficacy Rule represents a unique regulatory approval pathway to address drug development in situations where clinical efficacy studies are not ethical or feasible. This challenging and technically difficult strategy can only be applied in drug development when no other regulatory pathway is possible.
Do you need guidance in developing a product under the Animal Rule? We can help! Learn more about our clinical pharmacology services.



