February 3, 2026
The primary purpose of a clinical trial is to address a defined scientific hypothesis using the statistical method that aligns with the question at hand. Often, this hypothesis relates to the effect of one treatment compared with another. For example, you may compare the effectiveness of a new antibiotic to an established therapy. The statistical approach you choose should reflect the specific question you want to answer.
Using this antibiotic example, we can define three possible hypotheses:
- The New Antibiotic is at least as good as the Old Antibiotic (i.e., non-inferior)
- The New Antibiotic is better than the Old Antibiotic (i.e., superior)
- The New Antibiotic is equivalent to the Old Antibiotic (i.e., bioequivalent)
Though these hypotheses may sound similar, they represent distinct scientific questions and therefore require different analytical methods and trial designs.
Non-Inferiority
Tests whether the new antibiotic is not unacceptably worse than the current treatment, within a predefined margin (α):
New Antibiotic≥Old Antibiotic−α
Superiority
Tests whether the new antibiotic is statistically better than the current treatment:
New Antibiotic > Old Antibiotic
Bioequivalence
Tests whether the new and old antibiotic perform essentially the same, within a predefined margin (±α):
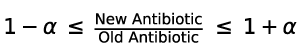
Each of these hypotheses has unique implications for sample size and trial outcomes. Non-inferiority typically allows for the broadest range of successful outcomes (equivalence or superiority) and usually requires a smaller sample size. Superiority trials, particularly when expected differences are modest, often require larger sample sizes. Bioequivalence trials are the most restrictive, demanding that treatments be effectively identical (not better or worse) within acceptable bounds, commonly ±20%, and therefore often require substantial participant numbers.
Which design is best?
That depends on the scientific question at the core of your program.
- Non-inferiority studies establish that a new therapy achieves at least the standard level of benefit and are common in comparative studies.
- Superiority trials are essential when demonstrating a clear benefit over placebo or when pursuing claims such as “our drug is better.”
- Bioequivalence trials are fundamental for generic drug and biosimilar approval, where equivalence to a branded reference product must be shown.
Making the right choice in trial design can mean the difference between a quick approval of a promising new therapy or incurring costly delays or even failures. That’s why leading development teams are increasingly using model-informed approaches to de-risk decisions and optimize design strategies.
At Certara, integrated methodologies like Model-Based Meta-Analysis (MBMA) and modern pharmacometrics (PMx) are transforming how development decisions are made:
- MBMA synthesizes clinical trial data across studies to quantify comparative efficacy and safety, inform differentiation targets, and support smarter trial design and competitive benchmarking.
- Recent industry collaborations and case examples show MBMA’s role in refining dose decisions, building synthetic control arms, and improving regulatory and strategic planning.
- Certara’s Expedited Pharmacometrics Regulatory Submissions offering now accelerates submission-ready PMx analyses, helping sponsors cut typical timelines by more than half, a testament to the central role of modeling in regulatory decision-making.
Together, these approaches help teams answer the key question you start with: Which hypothesis am I trying to address, and how can I design a trial that gets me there with the greatest probability of success?
Learn how to apply MBMA to strengthen your trial strategy
Download Certara’s guide: “MBMA vs. Meta-Analysis: Quick Comparison Guide”, to see how model-based meta-analysis outperforms traditional methods in predicting outcomes, informing trial design, and enabling more confident decision-making.
FAQs
What is the main difference between non-inferiority, superiority, and equivalence trials?
The difference lies in the scientific question being asked. Non-inferiority trials assess whether a new treatment is not meaningfully worse than an existing one within a predefined margin. Superiority trials test whether a new treatment is better than a comparator, while equivalence (bioequivalence) trials determine whether two treatments perform similarly within acceptable upper and lower bounds.
How do I decide which trial design is most appropriate for my program?
The optimal design depends on your development objective. Non-inferiority is commonly used to show comparable benefit to standard of care, superiority is needed to demonstrate clear differentiation, and bioequivalence is required for generics and biosimilars. Selecting the right design early is critical to avoid unnecessary cost and delays.
Which trial design typically requires the largest sample size?
Bioequivalence trials usually require the largest sample sizes due to the need to demonstrate similarity within tight margins. Superiority trials may also require large samples when expected treatment differences are small, while non-inferiority trials often allow more flexibility.
Can a non-inferiority trial also demonstrate superiority?
Yes. If a non-inferiority trial shows that the new treatment performs better than the comparator beyond the predefined margin, it may support a superiority claim, provided the study is appropriately designed and analyzed.
How can MBMA improve trial design and decision-making?
Model-Based Meta-Analysis integrates data across multiple studies to quantify treatment effects, reduce uncertainty, and inform realistic differentiation targets. This helps sponsors choose the right hypothesis, optimize sample size, and increase the probability of trial success.

Matt Zierhut, PhD MBA
Vice President, MBMA Capability Lead, Certara Drug Development SolutionsMatt advances the integration of published clinical outcomes data into development decisions and commercial and regulatory strategy via model-based meta-analysis (MBMA). Matt works closely with clinical development teams to ensure MBMA is leveraged for optimal impact when making the most critical decisions.

Erika Brooks
Marketing Director, Quantitative Science ServicesWith over 22 years of experience in hospitals, health systems, associations, life sciences, physician practices, and suppliers, Erika is an experienced marketing strategist and supports the Quantitative Science Services offering with Go-to market planning and execution.
This blog was originally published in 2011 and has been updated for accuracy.
Contact us